|
|||||||||
AbstractParapharyngeal acinic cell carcinoma is extremely rare. Surgical approaches to this space are quite difficult because of the highly important anatomical structures such as mandible, parotid tissue and major vessels.Parapharyngeal space (PPS) masses clinically diagnosed with late onset of symptoms. Magnetic resonance imaging is helpful in the distinction of parotid gland tumor from extra-parotid tumors. Transoral, transcervical, transmandibular and transparotid approaches are applied for surgery. This case reported 40 years old female patient with a painless growing mass in the neck. She had right sided, circular, well circumscribed hyperintense mass on the T1-and T2-weighted magnetic resonance imaging. Transcervical approach without mandibular osteotomy was applied to the patient. Pathology reported as a low grade acinic cell carcinoma. PPS is very difficult to access and requires high level of anatomical and surgical knowledge for treatment. IntroductionThe parapharyngeal space (PPS) is the reverse triangular space extending from the skull base to the hyoid bone and contains internal jugular vein, the carotid artery, cranial nerves and sympathetic nerve. This region has a wide variety of anatomical structures. Pleomorphic adenoma is the most common tumor of this space. Neurogenic tumors, lymphomas, and glomus tumors may also originate from this space [1,2]. PPS tumors are rare and account for only 0.5% of all head and neck tumors. Most of these tumors are benign lesions [1]. Acinic cell carcinoma is a low-grade malignancy constituting 3% of all salivary gland tumors and mostly occurs in the parotid gland. Surgery is applied for symptomatic tumors of this space. Surgical approaches are quite difficult because of the highly important anatomical structures such as mandible, parotid tissue and major vessels. Transcervical, transoral, transparotid and transmandibular approaches are the most widely used approaches [2]. This case reported an extra-parotid gland PPS tumor and discussed the surgical approach for the treatment. Case ReportA fourty years old female patient was admitted to the outpatient clinic with a growing mass in the neck. The mass was well-circumscribed, round and mobile in the parotid region without any symptom. There was no palpable cervical lymphadenopathy. Physical examination was otherwise normal. Flexible endoscopic examination of the larynx and pharynx was also normal. There were no neurological symptoms and signs. Coronal T1 and T2-weighted magnetic resonans imaging demonstrated a right sided well-circumscribed hyperintense mass medial to the parapharyngeal fat. Axial tomography revealed a 5x3 cm isointense PPS tumor. There wasn’t any invasion to the surrounding structures (Figure 1,2). No malignancy has been reported on fine-needle aspiration biopsy.
The informed consent was obtained from the patient. The resection of the tumor was performed by a transcervical approach without mandibular osteotomy. A modified Blair incision was performed as in parotidectomy. Parotid tissue was dissected from the sternocleidomastoid muscle. The submandibular gland was gently retracted medially while sternocleidomastoid muscle was retracted laterally to expose the digastric muscle (Figure 3).
Parotid gland and branches of the facial nerve were preserved. PPS mass was exposed between the posterior belly of the digastric muscle and the mandibula by transcervical approach. The tendon of the digastric muscle was resected for a better exposure (Figure 4). The non-invasive mass was dissected from the surrounding tissue. The lingual and hypoglossal nerves were preserved. There was no need for local flap for the closure of the wound. The patient recovered without any complication.
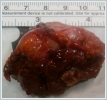
The pathologic examination reported 5x3 cm acinic cell carcinoma with encapsulated ovoid cells. There was no vascular or perineural invasion. Surgical margins were free of tumor. Patient had 6500 cGy radiotherapy postoperatively. There wasn’t any recurrence or metastasis in 4 years follow-up DiscussionParapharyngeal space masses clinically diagnosed with late onset of symptoms because of the deep location. The possible formation mechanism of the PPS tumors is the transformation of the residual minor salivary gland to malignant tissue in this fatty area. Parapharyngeal space tumors often present as a painless mass in the neck as in this case. PPS masses do not constitute shifting in the oropharyngeal structures until3 cmin diameter. Thus, PPS masses are diagnosed most of the time radiologically. But the radiology is still unable to differentiate benign and malignant disease. The contour of the mass can be helpful in diagnosis. Transparotid, transcervical, transoral or transmandibular approach can be applied in PPS masses. If the mass is originating from parotid gland, transparotid transcervical approach is applied. Otherwise transparotid approach is not applied to avoid facial nerve injury as we did in this case. The posterior belly of the digastric muscle can be resected if there is no adequate exposure to this space. The hypoglossal, accessory and lingual nerves should be preserved. However, they can be ligated in case of an invasion [3]. Total parotidectomy is the treatment in the deep lobe parotid gland tumors of the PPS and enucleation should never be done. Post-operative radiotherapy is recommended for the residual microscopic disease. The transmandibular approach can be applied for revisions, large lesions, and previous radiotherapy patients. Transoral approach is used in very small and limited tumors because of disadvantages. The most important disadvantage is the limited exposure. In contrast, transoral robotic surgery (the Da Vinci system) has a better vision and precision that offers a safe and efficacious transoral excision [4]. Transoral robotic surgery needs a very good knowledge of anatomy and special education. Anatomy is confusing and unusual for the surgeon. Transoral robotic surgery has recently been applied for tongue and supraglottic larynx cancers (5). Robotic surgery provides less blood loss, less pain and shorter hospital stays [6]. The surgical margins are very important in malignant tumors. The functional deficits such as swallowing and speaking may occur. Median mandibular osteotomy can be applied in malignancies that require extensive surgical resection. Mandibular osteotomy can also be applied for benign lesion when the exposure is not enough. In this case, the malignant tumor was resected without mandibulotomy because of adequate surgical exposure. Acinic cell carcinoma behaves as a low-grade malignant tumor and rarely metastasizes. The histological findings and the clinical course can be confusing. There are reported cases of low grade tumors which behave as aggressive tumors. The malignant tumor in our patient acted as a low-grade tumor and did not metastasize in 4 years follow-up. There is no definite method for the differentiation of the deep lobe tumor from extra-parotid tumor. The diagnosis can be made preoperatively by high-resolution magnetic resonance imaging. If there is a displacement in the parapharyngeal fat anteromedially, the tumor can be defined as extra-parotid mass. However, when the tumor is too large, it is difficult to differentiate the parapharyngeal fat leading to confusion about the origin of the tumor. This can lead to some difficulties in deciding the surgical approach. In our case, the parapharyngeal fat was easily defined and the tumor was completely extra-parotid mass. The low-grade tumors can sometimes behave as aggressive tumors. Patients should have radiotherapy in a poor prognostic histology. For this reason, our patient had radiotherapy although the tumor was reported as a low-grade tumor. PPS is a narrow space with important anatomical structures and it is not always easy to provide surgical margins. In this case report, radiotherapy was also applied to avoid recurrence as surgical margin was not enough. In conclusion, acinic cell carcinoma of the PPS is a rare tumor. It is very difficult to access and requires high level of anatomical and surgical knowledge for the treatment. References
|
|||||||||
| Keywords : Asinik hücreli karsinom , Parafaringeal bölge tümörü , Cerrahi | |||||||||
|