|
|||||||||
AbstractKlippel-Feil syndrome is a rare congenital deformity of the cervical vertebra. Short neck and limited neck movements are characteristic features of the syndrome, because of these features, a standard tracheostomy procedure is often difficult or sometimes impossible in these patients.A 9-month-old patient with Klippel Feil syndrome was decided to undergo tracheostomy for prolonged intubation. The patient's short neck and limited neck movements made a standard tracheostomy impossible. Tracheostomy was performed with a combined approach with partial sternotomy To our knowledge, this reported case is the youngest patient with Klippel Feil syndrome who underwent tracheostomy with this approach in the literature. IntroductionKlippel-Feil syndrome is a rare congenital deformity of the cervical vertebra. There is limited neck movement due to short neck, low hairline and fusion of at least two cervical vertebrae. Short neck and limitation of movement in the cervical vertebrae make it difficult to control the airway, if necessary, in these patients from birth [1]. In this case report, we would like to present tracheostomy with partial sternotomy in a nine-month-old patient with Klippel-Feil syndrome who was intubated and followed up in the intensive care unit. Case ReportA 9-month-old girl patient (Figure 1) was consulted to the otolaryngology clinic for prolonged intubation and with the request of performing tracheostomy for mechanical ventilator assisted palliative care at home.
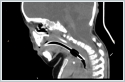
The patient’s short neck was noticed at the birth, but no further examination was performed. She was intubated with flexible fiberoptic endoscopy and taken to the intensive care unit for respiratory distress due to pneumonia after three months from the birth. Thorax and neck tomography of the patient revealed segmentation and formation anomalies at different levels in all cervical vertebrae and the first five thoracic vertebrae, cystic mass in the posterior mediastinum with radiological findings consistent with a neurenteric cyst, pleural effusion in basal segments of both lungs and pneumonia, and she was diagnosed with Klippel-Feil syndrome. The patient was operated by the neurosurgery department because of neurenteric cyst and a chest tube was inserted into the patient in whom chylothorax developed after the operation. Extubation was tried twice at one-month intervals during her follow-ups, but the patient was intubated again since she could not tolerate extubation. The patient followed up for the last three months and decided to perform tracheostomy with partial sternotomy due to the limitation of neck movements, short neck and beginning of the first tracheal ring at the sternal notch level on tomography (Figure 2).
Under general anesthesia, a 3-cm vertical skin incision was made in the midline from the upper limit of the neck to the sternal notch. The strap muscles were reached by passing over the skin, subcutaneous adipose tissue and platysma. The thyroid cartilage was seen at the bottom after the strap muscles were dissected and taken to the lateral side (Figure 3).
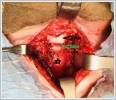
Dissection was continued to the inferior side over the thyroid cartilage. The lower limit of the cricoid cartilage was made visible by dissection, but this level was progressing below the sternal notch. The skin incision was extended to the inferior side in the midline in order to reach the tracheal rings. The sternum was reached after tissue dissection above sternum by passing over the skin and subcutaneous tissue. The sternum was cut 2 cm from the midline with bone scissors. At that time, thymus tissue was encountered and retracted to the lateral side. Wedge-shaped excision was performed from both upper sternal parts in order to increase the exposure and to facilitate cannula exchange in the postoperative period. After the sternal parts were retracted to the lateral side, the first three tracheal rings became visible (Figure 4).
After dissecting the perichondrium on the tracheal rings, the trachea was suspended with two non-absorbable 3/0 silk sutures that were passed between the first and second tracheal rings without damaging the inner mucosa of the trachea and the endotracheal tube. Needle at one end of the sutures were removed, both ends were taken out of the surgical site and fixed on the skin to be used in cannula exchange in the postoperative period. Subsequently, a vertical incision was made into the trachea between the second and third tracheal rings with #15 scalpel without damaging the endotracheal tube. Meanwhile, the anesthesiologist pulled the endotracheal tube up 2 cm, and the tracheostomy cannula was inserted into the tracheal passage. The ventilator was connected to the cannula, and the endotracheal tube was completely removed on the rise of patient's saturation above 95%. TRACOE silcosoft® Ref 373 (inner diameter of 3.5 mm, outer diameter of 5.4 mm, total length of 40 mm, proximal part length of 25 mm) silicon tube with cuff and long proximal part was preferred due to the patient’s being short necked and for easy postoperative cannula care. The cannula number was determined based on the patient's endotracheal tube size with an inner diameter of 3.5 mm. The neck band was sutured to the skin from both sides and the operation was terminated after subcutaneous and skin closure on the sternum. No postoperative complications were observed. The patient is still being followed up as mechanically ventilated in the intensive care unit (Figure 5).
DiscussionTracheostomy is frequently performed in children due to upper respiratory tract obstruction, prolonged intubation, congenital or acquired upper respiratory tract anomalies and the need for palliative care [2,3]. A standard pediatric tracheostomy begins with a neck incision between the cricoid cartilage and the sternal notch by extending the patient's neck, and ends with the insertion of the cannula following tracheal incision after reaching the trachea and seeing the tracheal rings [4]. However, this classical approach is not easy to perform in short necked children with cervical vertebral anomalies [5]. A classical tracheostomy could not be performed in our patient due to short neck and cervical vertebral anomaly caused Klippel-Feil syndrome. To our knowledge, there are no case reports or case series describing airway management with tracheostomy in children with Klippel Feil syndrome. In a case where an adult patient with Klippel Feil syndrome was presented, a tracheostomy was planned for the patient due to prolonged respiratory distress, but as in our case, they saw that the initial level of the trachea was below the sternum and they performed sternal resection to open the tracheostomy [6]. Biderman et al. described retrosternal percutaneous tracheostomy performed in 21 adult patients in whom standard tracheostomy was impossible to perform (7 patients with musculoskeletal deformation, 4 patients with hallow / C-spine fixation after neck injury or surgery, 7 patients with morbid obesity, 3 patients with goiter) [5]. We did not prefer this technique because our case was a child and we did not have any experience of percutaneous tracheostomy. It has been reported in the literature that tracheostomy-related mortal mediastinal infection may be observed in patients who underwent sternotomy for cardiac surgery [7]. In our patient, we did not encounter any infection in the postoperative period, and this may be due to partial sternotomy. However, long-term follow-up results are uncertain. A study comparing short and thick necks with normal necks has shown that the distance of the trachea from the skin increases as the structural problems of the cervical spine increase [8]. When choosing a cannula for our patient, we preferred a longer cannula than the normal cannulas designed for this age group because these cannulas are often incompatible for obese patients and short-necked persons as normal anatomic criteria are taken into account when standard cannulas are designed [9]. Conclusion When tracheostomy is required in short-necked patients with limitation of movement in the cervical vertebrae such as Klippel-Feil syndrome, a combined approach with partial sternotomy may be preferred instead of the classical tracheostomy approach. When selecting the cannula, a longer cannula should be selected than the standard cannulas. References
|
|||||||||
| Keywords : Klippel Feil sendromu , pediatrik trakeostomi , uzamış entübasyon , kısa boyun , sterotomi | |||||||||
|