|
|||
AbstractSynovial sarcoma is a malignant and highly aggressive soft tissue tumor. It commonly arises from extremities and it is very rare in head and neck region. Primary synovial sarcoma of the head and neck region constitutes only 2% of all synovial sarcoma cases. A 43-year-old male was admitted to our clinic with the complaint of a mass in left parotid gland region persisting for 2 months. According to imaging studies and biopsy result, total parotidectomy operation with preservation of facial nerve was performed. Histopathological investigation was compatible with synovial sarcoma and diagnosis was confirmed with fluorescence in situ hybridization analysis. We aimed to present a very rare case of primary monophasic synovial sarcoma of the parotid gland and discuss the importance of fluorescence in situ hybridization analysis in differential diagnosis.IntroductionSynovial sarcoma (SS) is a malignant soft tissue tumor and comprises 5-10% of all soft tissue sarcomas. It is accepted as a slowly growing but highly aggressive tumor and mostly arises from the extremities of adolescents and young adults [1]. In the head and neck region, primary SS is very rare and only constitutes 2% of all SS cases. Furthermore, if it occurs in this site, biphasic synovial sarcoma tends to be more common than monophasic type [2]. In this study, we present a very rare case of primary monophasic type synovial sarcoma of the parotid gland with review of the literature. Case ReportA 43-year-old male was admitted to our clinic with the complaint of a mass in the left parotid gland region persisting for 2 months. In the physical examination of the patient, a palpable mass possibly located in the deep lobe of the parotid gland was palpated. There was no other palpable lesion in the neck and pan-endoscopic examination revealed no abnormality. A computed tomography (CT) scan was performed. CT scans showed 25 x 17 mm sized soft tissue mass originating from the deep parotid lobe.
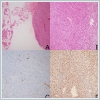
A fine needle aspiration biopsy (FNAB) was performed and cytopathology was reported as salivary gland neoplasm of uncertain malignant potential (SUMP). According to this report, left total parotidectomy with preservation of facial nerve operation was performed. On histopathologic examination, spindle-shaped malignant cells around the parotid gland were observed.
With immunohistochemistry analysis, Cytokeratin 19 positivity and TLE1 expression were reported (Figure 2C-2D). After that synovial sarcoma was suspected and for the confirmation of the diagnosis fluorescence in situ hybridization (FISH) analysis was performed. FISH analysis signal pattern was consistent with SS-18 gene rearrangement. The diagnosis was monophasic synovial sarcoma and the patient referred to radiation oncology and received adjuvant radiation. At 12 months after the treatment, the patient is well without evidence of recurrence. DiscussionThe tumors arising from the salivary gland are commonly located in the parotid gland (80%). Second most common site is submandibular glands while sublingual and minor salivary glands are less frequently involved [3]. Although most of the tumors originating from the parotid gland are benign, malignant tumors are also common (20 %) and most common malignant tumors are mucoepidermoid carcinoma and adenoid cystic carcinoma. Also, there is a small group of non-epithelial tumours which are commonly benign, comprise 5% of all salivary gland neoplasms. This group includes haemangioma, lipoma, neuromas, neurofibromas, lymphoma and sarcomas [4]. Parotid gland tumors usually originate from superficial lobe and tumours involving exclusively the deep lobe are very rare. The role of FNAB in the differential diagnosis of parotid tumors is very important. However, it is not always easy to determine malignant tumor subtypes and tumor grades with FNAB [5]. For the standardized terminology to replace conventional interpretation for salivary gland cytopathology Milan System for Reporting Salivary Gland Cytopathology (MSRSGC) was established. According to this classification system, FNAB results divided into 7 categories: non-diagnostic (category I), non-neoplastic (category II), atypia of undetermined significance (AUS) (category III), benign neoplasm (category IVa), salivary gland neoplasm of uncertain malignant potential (SUMP) (category IVb), suspicious for malignancy (category V), and malignant (category VI). The SUMP category defines a group of cases with diagnostic for neoplasm but indefinitive for a specific tumor type to further distinguish between benign or malignant. The risk of malignancy for SUMP cases was reported to be 35% and surgery was recommended for the treatment of these cases [6]. SS is a malignant soft tissue tumor and mostly originates in proximity to large joints and bursae of the lower extremities such as the knee, tendon sheaths, and bursal structures but it is very rare in the head and neck region [7]. In this area, the most common sites are hypopharynx and parapharyngeal spaces [4]. Two subtypes of SS are described: monophasic type which contains spindle cells and biphasic type which includes both spindle cells and well- developed glandular epithelial structures [8]. Histopathological diagnosis of SS is generally very difficult not only with haematoxylin and eosin stain but also with various immunostaining techniques. But in recent years it has been shown that more than 95% of SS harbor the specific chromosomal translocation, t(X;18)(p11.2;q11.2), which generates SS18-SSX1, SS18-SSX2, and rare SS18-SSX4 fusion proteins. Based on these findings FISH analysis started to be used for the accurate diagnosis of the SS. The SS18 break-apart dual-color signal probe, designed to label the sequences adjacent to SS18 on chromosome 18, is the most common and widely applied probe in FISH analysis [9]. In our case, after histopathologic suspicion of SS, we performed FISH analysis and SS diagnosis was confirmed by molecular pathologically. We believe that FISH analysis method is very contributive and should be included as the gold standard method for differential diagnosis. In the management of these tumors, multimodal approach was recommended. Radical surgery and adjuvant radiotherapy is the most appropriate treatment method. Chemotherapy with ifosfamide has been tried in some cases. But there is limited data on literature for the management of head and neck synovial sarcoma due to the low incidence in this site [10]. The prognosis of these tumors varies. Al- Daraji et al. analyzed 36 SS cases involving head and neck region in their study and reported that prognosis seems relatively good for those patients whose tumor size is less than 5 cm, contains fewer than 10 mitoses/10 high-power fields, and is devoid of a poorly differentiated component [2]. Primary monophasic synovial sarcoma of the parotid gland is a very rare entity. The rarity of these tumors in the head and neck region makes differential diagnosis quite difficult. For these reasons, FISH analysis method has very crucial role and it has to be used in suspicious cases. References
Presented at41th Turkish National Congress of Otolaryngology Head and Neck Surgery, Antalya, Turkey. |
|||
| Keywords : sinovyal sarkom , floresan in situ hibridizasyon , parotis sarkomu | |||
|