|
|||||||
AbstractWe describe a case of larynx squamous cell carcinoma (SCC) with severe stenotic atherosclerotic carotid artery disease (ASCAD) in a 59-year-old male patient. The patient underwent simultaneous carotid endarterectomy and oncologic surgery without any complications. Oncologic surgery for larynx SCC and carotid endarterectomy may be performed simultaneously without additional morbidity at the same procedure in selected patients.IntroductionAtherosclerotic carotid artery disease (ASCAD) and squamous cell carcinoma of the head and neck (HNSCC) can be simultaneously present, having identical risk factors including age, sex, smoking, alcoholism, irradiation, and occupation [1]. Surgery and/or irradiation for HNSCC and cancer-associated hypercoagulation can also contribute to cerebrovascular accidents and ASCAD during treatment of the primary tumor [2,3-6]. Here, we describe a case of larynx squamous cell carcinoma (SCC) with severe stenotic ASCAD who underwent simultaneous carotid endarterectomy and oncologic surgery. Case ReportA 59-year-old male patient presented with a history of intermittent hoarseness persisting for about a year. In the last few months, he had progressive dyspnea with mild dysphagia. He had an 80 pack-year history of smoking with no alcohol consumption. Endoscopic examination of the larynx revealed a lesion of the left true vocal cord extending to the interarytenoid and subglottic area with a left vocal cord immobility (Figure 1a). There were no palpable lymph nodes in the neck.Contrast-enhanced larynx CT of the patient demonstrated a tumoral lesion of the left subglottic area extending through the left vocal cord with anterior commissure invasion (Figure 1b).
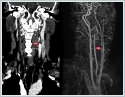
There was also severe stenosis of the left internal carotid artery (Figure 2a). Doppler ultrasonography and 3D contrast-enhanced MR angiography (Figure 2b) revealed a focal severe stenosis (70-99%, according to the NASCET criteria [9]) of the left internal carotid artery, located one centimeter above the carotid bifurcation. The patient was free of any symptoms regarding stenosis of the carotid artery.
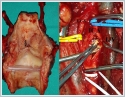
Direct laryngoscopy and biopsy were performed after securing the airway with tracheotomy. Direct laryngoscopy demonstrated a tumoral lesion of the left subglottic area, invading the left true vocal cord, ventricle and interarytenoid area. The subglottic extension of the tumor was more than one centimeter and histopathological examination of the punch biopsies taken from the left vocal cord, subglottic and interarytenoid area revealed SCC of the larynx. After consultation with a vascular surgeon, total laryngectomy (Figure 3a), bilateral lateral neck dissection and simultaneous carotid endarterectomy (Figure 3b) were performed on the patient at the same procedure.Total laryngectomy was performed to the patient due to involvement of the interarytenoid area with extensive left subglottic tumoral disease.
The postoperative course was uneventful but histopathological examination revealed a metastatic lymph node of level IV on the left side of the neck and thyroid cartilage invasion. The patient received adjuvant radiotherapy to the primary tumor bed, peristomal area and bilateral level II-VI lymph nodes. A Doppler study following the completion of adjuvant radiotherapy revealed a patent carotid artery and close follow-up of the patient is ongoing. DiscussionASCAD is a serious condition that causes a risk of stroke with stenosis of the carotid artery due to the progression of atherosclerosis with time. The risk of stroke is correlated with the percentage of carotid stenosis [1]. The prevalence of hemodynamically significant carotid stenosis (>50%) in the general population is between 1.2% and 4.2% [7,8]. The treatment of advanced ASCAD can be done either medically or surgically. Medical treatment includes anticoagulation therapy, diet and hyperlipidemia control. Surgical therapy involves a carotid endarterectomy. The North American Symptomatic Carotid Endarterectomy Trial revealed that surgical treatment offers better results than medical therapy for symptomatic stenosis greater than 70%, with an absolute reduction in stroke risk of 9% versus 26% [9]. On the other hand, treatment of asymptomatic ASCAD is not very clear. The Asymptomatic Carotid Atherosclerosis Study demonstrated a reduction of 1% in morbidity and mortality with surgical treatment in patients with asymptomatic carotid stenosis of 60% or greater [10], and therefore many clinicians have advocated a watch-and-wait approach [5]. ASCAD and HNSCC have similar risk factors that provide a major concern in the co-existence of these pathologies. Age, sex, smoking, alcoholism, irradiation, and occupation are identical risk factors of the two pathologies [1]. Although similar risk factors may contribute to the co-existence of ASCAD and HNSCC, Cote et al [1] reported that the rate of carotid disease in patients with HNSCC was similar to that found in the general population. Nevertheless, there are very few reports in the literature regarding combined oncologic resection and carotid endarterectomy in patients with HNSCC. Rechtweg et al [11] reported three patients who underwent neck dissection for HNSCC and simultaneous carotid endarterectomy. They concluded that endarterectomy for severe carotid stenosis can be performed simultaneously with treatment of HNSCC with no increase in morbidity. In their series of 11 patients, Kroeker et al [12] found that the collaboration of head and neck surgeons with vascular surgeons provides the patient with oncologic resection and revascularization with a low perioperative risk of stroke. In the present case, simultaneous oncologic surgery and carotid endarterectomy were achieved without any complication in the patient with larynx SCC and severe stenotic ASCAD. The excellent visualization of the carotid artery during the neck dissection facilitated the removal of atherosclerotic disease localized in the internal carotid artery with minimal surgical risk by the vascular surgeon. Patients with simultaneous HNSCC and severe stenotic ASCAD may benefit from combined oncologic surgery and carotid endarterectomy in the same procedure to prevent cerebrovascular disease that may occur peri- or postoperatively owing to the untreated ASCAD. Nevertheless, larger series with more participants are required to definitely establish the safety and potential risks of the combined procedure. Conclusion Oncologic surgery for larynx SCC and carotid endarterectomy may be performed simultaneously without additional morbidity at the same procedure in selected patients. AcknowledgementThe authors thank Dr. Alper Sami Kunt from the Department of Cardiovascular Surgery, Kayseri Training and Research Hospital, for his assistance in the procedure of carotid endarterectomy. References
|
|||||||
| Keywords : Larenks , Karsinom , Yassı hücreli , Endarterektomi , Karotis | |||||||
|