|
|||
AbstractThree - year old girl who applied to ophthalmology due to the complaint of bilateral exotropia and had bilateral giant ethmoid mucocele detected by CT scan was referred to our otolaryngology clinic. According to the patient’s medical history, she was followed up due to diagnosis of cystic fibrosis, a sweat test was conducted to confirm that the diagnosis was positive, and a N1303K mutation was identified based on a genetic test. Finally, endoscopic bilateral mucocele marsupialization was performed to the patient.Introduction
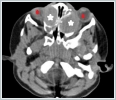
This disease emerges due to the mutation of a gene that codes cystic fibrosis transmembrane regulator protein (CFTR) in chromosome 7q31. While more than 2000 mutations have been identified on the gene sequence that codes CFTR (Retrieved from www. genet. sickkids.on.ca/cftr) the most prevalent mutation is F508del and it contains 70% of defective alleles. This gene was first described in 1989, codes a protein that works as a chloride channel. Also, its dysfunction causes abnormal sodium and chloride transportation throughout the apical membranes of front aerodigestive tract epithelial cells and exocrine glands. Abnormal salt and water flow cause dehydration of exocrine glands and change in the viscoelastic features of mucin excretion. Nasal and paranasal sinus diseases occur in almost all CF patients and complaints based on chronic sinusitis or/and nasal polyposis are emerged in nearly 40% of patients who are above 5 years old [3]. A limited number of cases have been reported regarding ear, nose, and throat (ENT) pathologies for CF patients; thus, there is insufficient information about nasal and paranasal sinus involvement in the first years of their life [4-6]. Life quality indicator of sinus disease reflects pulmonary functions, especially for children, and shows that it could be a determinant of pulmonary disease. Until 30 years ago, sinus illness causes death generally in the first decade of life due to pulmonary defect based on the opportunistic infection. The improvements of the treatment have explicitly provided that the current median life expectancy has increased the survival up to 36.8 years [7]. The viscosity of mucus stasis that emerged from sinuses is responsible for intraluminal retention, obstruction of the ostium, chronic sinus inflammation, and superinfection. Mucoceles, however, one of the best-known complications of chronic sinusitis for adults, and it is a rare complication for children. The mucoceles are cystic forms that secrete mucus filled with respiratory epithelium and show slow concentric expansion. They are benign in nature, however, they may also enlarge due to accumulation of secretion and they may cause local, orbital, or intracranial complications by pushing, eroding, or melting bony structure around them [8]. This study aimed to report a 3-year-old girl who has bilateral ethmoid mucocele that causes two-sided orbital complications related to very rare cystic fibrosis and was to discuss the pathology of sinonasal involvement. Case ReportDue to the presence of epiphora in her eyes, proptosis, limited eye movement, diplopia, and exotropia, a three-year-old girl patient who applied to ophthalmology were referred to our Ear, Nose, and Throat (ENT) clinic because of having lesions compatible with mucocele in her paranasal Computed Tomography (CT) scan. The parents of the patient realized limited eye movement of the patient since she was 1 year old; thus, they applied to ophthalmology. The patient had also a complaint of stuffy nose and runny nose, and a standard ENT examination was performed and an endoscopic evaluation of the nose was performed. Bulging and thick mucoid secretion were observed at the nasosinusal walls of both nasal cavities. She also has bilateral exophthalmos and exotropia. Based on the patient’s medical history, her sweat test, which was first conducted when she was 8 months, was positive and she was being followed up by the pediatric department because of a cystic fibrosis diagnosis. Also, a homozygote N1303K mutation on Exon 24 of CFTR Gene was detected based on her genetic screening at her follow-ups. The patient’s coronal and axial plane of CT scans revealed the presence of two homogenous and benign lesions whose borders were measured as about 28x18 mm for right and were not clear with the ophthalmic fissure, and 38x23 mm for left, and well-defined. We observed that they pushed medial rectus muscles throughout bilateral medial extraconal space and pushed partially the bulbus oculi in the lateral direction, and narrowed the nasal cavity, as well as in the left, protruded to retroorbital space, and eroded the sphenoid bone corpus (Figure 1), (Figure 2)
The proptosis of the patient was improved in the postoperative stage and eye movements were unrestricted in any direction. Nasal obstruction was improved and its rhinorrhea discontinued. Reoccurrence of mucocele was not observed during 18 months follow up period. However, the patient applied to our clinic due to complaints of a stuffy and runny nose during that 18 months period. After the endoscopic examination, polyps and mucopurulent secretion were observed in both middle meatuses. Therefore, antibiotherapy was started, and the patient also used nasal steroid and nasal hypertonic saline solutions. During the follow-ups, no sinusitis attacks were presented; polyps were observed in the middle meatus but these were not at the level of causing serious nasal obstructions. No treatment was advised at this asymptomatic stage. Follow-ups are continued during periodic intervals. The parents of the patient were informed about the operation and an informed consent form was assigned so that it could be written as a case report DiscussionNasal and paranasal sinuses' involvement in cystic fibrosis basically emerges as chronic sinusitis and nasal polyposis. The nasal polyposis is the first rhinology manifestation that is described for cystic fibrosis. Paranasal sinus mucocele is a rare condition for pediatric patients and the occurrence of this disease for pediatric patients with cystic fibrosis is unknown. While sinonasal mucoceles of the adult population are mostly observed in the frontal sinus, pediatric mucoceles are mostly observed in the ethmoid and maxillary sinuses. Di Cicco et. al reported that in the study involved 242 cystic fibrosis patients, the mucocele occurrence was 16.4% among the patients who had upper respiratory tract symptoms, and who scanned paranasal sinus CT. In this study, the occurrence of mucocele for patients with cystic fibrosis was 3.7%. In the same study, it was reported that 5 of the mucoceles were bilateral maxillary, 1 of them was unilateral maxillary, and 3 of them were maxillary and ethmoid mucocele [8]. Nicholas R. et al reported that 6 out of the 59 (10%) patients with cystic fibrosis who received endoscopic sinus surgery had mucocele. In the same study, they reported that all patients with mucocele had sinonasal polyposis. It was also reported that 4 of the 6 patients had unilateral ethmoid, 1 had maxillary and ethmoid, and 1 had frontal mucocele [9]. Thome et al. recruited patients with cystic fibrosis and ethmoid mucocele reported until 2000 and the sinonasal polyp rate was 40% among these cases. In this study, there were 10 patients, and among them, 6 patients had unilateral ethmoid, 2 patients had ethmoid and maxillary, and 1 patient had ethmoid, maxillary, and frontal mucocele altogether. In this study, Thome et al. also reported their own cystic fibrosis and bilateral ethmoid mucocele cases [10]. These studies are limited in the literature indicating that bilateral mucoceles mostly settle in the maxillary sinus, while ethmoid mucoceles tend to be located in one site. Our study is the second case in the literature reporting cystic fibrosis and bilateral ethmoid mucocele. Although the patient had not had sinus polyps during her first examination and surgery, sinonasal polyposis developed during her follow-ups. The rate of developing sinonasal polyps in cystic fibrosis patients increases with aging [8]. The existence of chronic nasal obstruction, nasal congestion, persistent mouth breathing, and nocturnal oxygen desaturation in cystic fibrosis patients suggests the possible presence of serious sinonasal pathologies like nasal polyposis and mucocele. Moreover, the presence of ophthalmologic symptoms such as epiphora, exophthalmos, and restricted eye movements along with chronic nasal obstruction is an early-sign of mucocele. Although paranasal sinus mucoceles are generally benign lesions, they cause surrounding bony structure erosion more frequently than expected [8]. Therefore, early diagnosis and treatment of mucoceles are critical before they lead to more severe complications. The reported patient herein was 3 years old and was referred to the ENT clinic for the first time. Therefore, the delayed diagnosis might cause that Orbita symptoms-related to mucocele were apparent, and might lead to dramatically enlarged mucocele dimension. Endoscopic nasal examination and paranasal sinus CT scans are the primary methods for the assessment of sinonasal involvement in cystic fibrosis patients. Magnetic resonance imaging (MRI), on the other hand, has a disadvantage for imaging bone structure and does not recommend for the pre-operative period [10]. There is no guidance showing which cystic fibrosis patients should refer to CT scanning. In general assessment of sinonasal symptoms, paranasal sinus CT is recommended for avoiding unnecessary radiation exposure of the patients, and it is upheld that CT scan should be limited to the pre-operative period if a surgical operation is planned. Surgical operations are inevitable for the following conditions: non-regressing sinusitis and/or polyposis in nasal obstruction and rhinorrhea despite conservative treatment, the presence of an apparent bulging at lateral nasal wall causing nasal obstruction during the endoscopic examination, and the presence of ophthalmologic symptoms such as epiphora, exophthalmos, and restricted eye movements. Besides, facial pain and headache-causing a decrease in life quality and pulmonary exacerbations corresponding to sinus symptoms are other conditions requiring a surgical operation. When such conditions exist, CT-based assessment can be a good approach. Paranasal CT assessment can also provide information in the case of nasal congestion that cannot be explained by the symptoms based on physical examination. Non-persistent rhinorrhea and polyposis which do not cause an explicit nasal obstruction or which is shrinking with medical treatment can be observed without CT assessment. In this situation, mucoceles causing complications because of bone erosion and asymptomatic condition may not be diagnosed properly. However, there has been no such case reported in the literature so far. A proper diagnostic procedure and timing of surgery are critical to prevent local and systematic complications. For example, cystic fibrosis patients at later ages may face a permanent nasal bone deformation seen in diplopia, pyomucoceles, or Woaks syndrome. On the other hand, mucoceles formation is thought to more likely begin with the intrauterine period since case reports are showing that infants were even diagnosed at the first months of their life [8]. Endoscopic drainage is accepted as a gold standard for the surgical procedure of mucoceles. Polyps and chronic sinusitis can be followed-up with conservative medical treatment. Gysin et al. showed that daily nasal irrigation with the normal and hypertonic solution or using local anti-inflammatory medicine works well for these patients [3]. During the latest follow-up visit of the patient, we reported herein, polyps and a trace of mucopurulent secretion were observed in the middle meatus. We prescribed low-dose corticosteroid drop and recommended nasal irrigation with saline solution and another follow-up visit. Generally, the mutations that ruin the function of the cystic fibrosis transmembrane conductance regulator (CFTR) gene cause cystic fibrosis. More than 2000 mutations have been reported and the most prevalent one is ∆F 508 mutation [11]. When the relationship between mutations and sinonasal involvement is considered, more occurrence rate of ∆F 508 mutations for patients with sinonasal involvement has been reported [12]. The CFTR gene is placed at the long arm (7q31.2) of chromosome 7 and it has 27 exons. For CFTR, all 27 exon regions must be healthy [11]. Homozygote N1303K mutation was detected at the CFTR gene Exon 27 in the study of genes for our case. This mutation was one of the classic mutations that cause cystic fibrosis as advised by the American College of Medical Genetics (ACMG) [11]. Other entities that cause mucocele signs and symptoms such as meningocele, rhabdomyosarcoma, hemangioma, and neuroblastoma must be eliminated [5]. Sinus mucocele should be considered in case of relapsing allergic conjunctivitis refractory to medical management particularly in patients with underlying systemic diseases such as CF [13]. Mucoceles can also cause proptosis and hypertelorism [14]. Additionally, mucoceles might cause strabismus. As a matter of fact, bilateral exotropia was also existed in our case along with diplopia and exophthalmos. In conclusion, during cystic fibrosis patients’ follow-ups, assessment of eye movements besides sinonasal symptoms is very important to diagnose mucocele complications. Mucocele complications should always take into consideration for especially patients with strabismus. If the patients have possible symptoms-associated with cystic fibrosis complications, these patients should immediately be examined by an ENT specialist. These examinations are critical due to the possible serious consequences of the complications. References
|
|||
| Keywords : Mukosel , kistik fibroziz , ekzotropi | |||
|