|
|||||||
AbstractExtramedullary plasmacytoma constitutes 3% of plasma cell neoplasms and is named according to location. Extramedullary plasmacytoma constitutes less than 1% of all head and neck malignancies and most frequently involves the respiratory mucosa in the head and neck region. Patients may present with different symptoms such as nasal congestion, epistaxis, rhinorrhea, sore throat, and dysphonia depending on the localization of the mass. In this article, a 60-year-old male patient diagnosed with maxillary sinus extramedullary plasmacytoma with orbital invasion is presented.IntroductionPlasma cell neoplasms are classified into the following three categories: multiple myeloma (MM), solitary plasmacytoma of the bone, and extramedullary plasmacytoma (EMP). Among these diseases, MM is the most common plasma cell neoplasia, which primarily not only involves the skeletal system but also metastasizes of the skeletal system [1]. EMP constitutes 3% of plasma cell neoplasms and is named according to its localization [2]. EMP accounts for <1% of all head and neck malignancies; furthermore, respiratory mucosa is most frequently involved (80%) in this region, and the nose and paranasal sinuses are most common sites of malignancy in the respiratory mucosa (75%) [3-5]. Patients may present with different symptoms such as nasal congestion, epistaxis, rhinorrhea, sore throat, and dysphonia depending on the localization of the mass [6-7]. A diagnosis can only be established after pathologically examining a biopsy taken from the mass [5]. In this article, we present the case of a 60-year-old man diagnosed with extramedullary plasmacytoma of the maxillary sinus with orbital invasion. Case ReportA sixty-year-old man visited our clinic with complaints of watering in the left eye, nasal congestion, and purulent nasal discharge approximately 1 month prior to the start of this investigation. Endoscopic examination revealed an ulcerovegetan mass in the left nasal cavity, the surface of which was covered with purulent secretions and desiccation. Paranasal computed tomography (PNCT) imaging of the patient revealed a lesion with a soft tissue density of approximately 4.2 × 4.4 × 5.3 cm in the left maxillary sinus, which caused extension in the anterior, medial, and lateral maxilla and the ceiling of the maxilla; furthermore, it was accompanied by thinning of the bony structure in the periphery. The medial wall of the maxillary sinus was eroded. Mild exophthalmos was observed in the left eye due to compression of the left orbital floor. The fat plane showed a faded appearance between the inferior rectus muscle and the lesion (Figure 1).
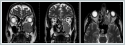
Contrast-enhanced facial magnetic resonance imaging of the patient showed T1 hypointense, T2 hyperintense, 5 × 4 × 3 cm lobulated contoured mass in the left maxillary sinus extending medially to the nasal cavity and left posterior ethmoidal cells. The mass also extended to the retromaxillary fat pad (Figure 2)
A biopsy from the maxillary sinus was planned for the patient under general anesthesia. The left middle meatus was dominated with the aid of a zero-degree endoscope. After uncinectomy, multiple punch biopsies were taken from the mass that nearly filled the maxillary sinus and extended from the maxillary sinus ostium to the middle meatus. Histopathological examination revealed a diffuse neoplastic plasma cell infiltration with an immunohistochemically kappa light chain monotype, showing focal CD3 expression (Figure 3).
The outcomes of a bone marrow aspiration biopsy performed on the patient were normal. No extralesional mass was observed in the PET/CT (Positron Emission Tomography–Computed Tomography) examination. The patient was diagnosed with extramedullary plasmacytoma with the present findings. Radiation oncology was consulted and radiotherapy was planned for the patient. DiscussionEMPs are malignant mass formations in soft tissue caused by monoclonal plasma cell proliferation [7]. They are 3 times more common in men than women and are especially seen in individuals aged 40–70 years; however, information related to their etiology is lacking. Since tumors originate from mucosa-related lymphatic tissue, inhaled allergens and chronic exposure to viral agents may have a role in their etiology [8]. EMP is typically diagnosed made by examining deep tissue biopsies from the mass owing to the fact that these tumors are localized in the submucosal region [8,9]. The clinical picture can vary depending on tumor localization. The most common clinical findings are soft tissue swelling and nasal congestion, whereas less common and nonspecific initial clinical findings include epistaxis, pain, proptosis, cervical lymphadenopathy, and cranial nerve paralysis [3]. We noted the presence of orbital invasion in our case with the EMP originating in the maxillary sinus. Although there was no restriction in eye movements yet, our patient had complained of watering in the left eye and nasal congestion. MM is reported in 10% of patients with masses that are initially considered as plasma cell infiltration [4]. Therefore, systemic involvement must be investigated after the diagnosis of plasmacytoma. Anamnesis, physical examination, complete blood count, serum protein electrophoresis, urine analysis for myeloma protein and bone marrow biopsy are recommended to perform differential diagnoses (Table 1) (10). PET-CT is a reliable and recommended method especially in the investigation of extramedullary disease and plasmacytoma. In our case, a diagnostic bone marrow biopsy was performed and was reported as normal. In addition, whole body scan was performed with PET-CT and no extralesional mass was observed. ( Table 1)
EMP is staged according to lymph node involvement [5,11]. Stage 1 is used to describe cases when the tumor is restricted to its primary location, Stage 2 when there is local lymph node involvement, and Stage 3 when there is metastatic spread. Lymph node involvement can be observed in 15%– 25% patients. However, presence of lymph node metastasis does not indicate poor prognosis [5]. Lymph node involvement was not observed in our patient, and the patient was categorized as Stage 1. Plasmacytomas are radiosensitive tumors. Treatment responses of local radiotherapy and surgery are similar [6, 12]. For EMPs, radiotherapy is recommended in cases of postsurgical margin positivity. Patients are typically directed to radiotherapy because of the difficulty of surgical excision of EMPs in the head and neck region [13]. Furthermore, >70% of EMP patients have a good prognosis and an average life expectancy of >10 years [14]. EMPs are rarely seen in the head and neck region. Because of its localization, patients first present their symptoms to an Otorhinolaryngologist. When a pathological diagnosis is made, it is imperative to evaluate the patient in terms of systemic disease, and long-term follow-up should be performed. References
|
|||||||
| Keywords : Ekstramedüller plazmasitom , maksiller sinüs , orbital invazyon | |||||||
|