|
|||
AbstractDiffuse large B cell lymphoma (DLBCL) is the most common non-Hodgkin type lymphoma that can be found localized in various extranodal sites. Nasal vestibule involvement is rare. In the follow-up of a 64-year-old female patient who presented to the Otorhinolaryngology (ENT) outpatient clinic for right nostril obstructing mass lesion starting about a month ago, complained of drowsiness. The Brain Magnetic Resonance Imaging (MRI) of the patient, in which the mass was also demonstrated in Paranasal Sinus Computed Tomography (PNS CT) scan, showed a contrast-enhancing mass lesion located superior to the left basal ganglion. Syndrome of Inappropriate ADH secretion (SIADH) was detected in laboratory tests. Radiotherapy was administered to the patient diagnosed with Diffuse Large B Cell Lymphoma on histopathological examination of the nasal vestibule biopsy. The diagnosis of a sinonasal DLBCL case presenting with SIADH is discussed.IntroductionApproximately one third of extranodal lymphomas are seen in the head and neck region. It is most commonly seen in the Waldeyer ring but can also appear in the sinonasal cavity [1]. 75% of extranodal nasal lymphomas have been detected as T-cell lymphoma while 25% as B-cell lymphoma [2]. Diffuse B-cell Lymphoma[DLBCL] is a rare non-epithelial malignant tumor of the nasal cavity and paranasal sinuses [3]. It is a rapidly growing lymphoma type and patients experience symptoms such as epistaxis, nasal congestion, visual impairment, hearing loss, weight loss, and fever. Neurological symptoms are more prominent in cases of central nervous system involvement [4]. To the best of our knowledge, there is no lymphoma case involving nasal vestibule present in literature. This case report presents a 64-year-old female patient with right nasal vestibule localized and central nervous system involved DLBCL. Case ReportA 64-year-old female patient with a complaint of an ulcerated, crusted lesion located in the right nasal vestibule, which started about 1 month ago and showed progressive growth, was admitted to the ENT outpatient clinic. The patient reported no other complaint apart from the lesion and in the physical exam, an ulcerated, crusted 3x3 cm mass in the right nasal vestibule that deviated to the left in the columella and obliterated the right nostrils almost completely was observed (Figure 1).
In the flexible endoscopic examination, the nasal cavity posterior to the right nasal vestibule, the left nasal cavity, nasopharynx, oropharynx, hypopharynx and larynx were unremarkable. No palpable mass was observed in head and neck examination. The patient had concomitant conditions such as autoimmune hepatitis, type II Diabetes Mellitus and Hypertension. Laboratory examination revealed Na: 116mEq / l, Cl: 77 mEq / l, BUN: 7mg / dl, Uric Acid: 2.8mg / dl, CRP: 145mg / l, LDH: 285 U / L, Erythrocyte sedimentation rate: 70 mm / hour. Complete urinalysis detected urinary Na of 59mEq / l value. In serological tests, TORCH panel was reported as negative, EBV EBNA: positive, EBV VCA IG M: negative, EBV VCA IG G: positive. Hemogram and other biochemical examinations were within normal limits. Neck ultrasonography (USG) and paranasal sinus computed tomography (PNS CT) imaging was performed. No additional pathology was found in the bilateral cervical region on USG. PNS CT scan revealed a soft tissue mass measuring 40HU in density, totally obliterating the right nasal vestibule, measuring ~ 29x26 mm in the widest area in the anterosuperior axial plane of the maxillary bone, that could not be clearly demarcated with surrounding soft tissues, not causing erosion or destruction of bone, and not having significant contrast enhancement (Figure 2).
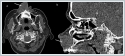
Failure of Na values to improve despite intravenous 0.9% isotonic replacement for hyponatremia, elevated urine sodium values, presence of hypouricemia and absence of edema and dehydration signs led to the diagnosis of Syndrome of Inappropriate ADH secretion (SIADH). Contrast-enhanced brain Magnetic Resonance (MRI) and diffusion MRI imaging was performed to assess central pathologies due to the presence of drowsiness, poor general condition and SIADH. In contrast-enhanced brain MRI imaging, in addition to bilateral frontoparietal nonspecific white matter lesions, another round mass lesion with a size of 21 * 18 mm at the level of the left basal ganglion superior, T1A hypointense, T2A hyperintense, slightly enhancing after intravenous contrast medium, mild restricted diffusion was observed in the Diffusion MRI (Figure 3).
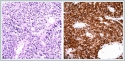
A wound culture was sent from the crusted area over the lesion and deep soft tissues in the biopsy material. Yeast cells and hyphae elements were reported in the culture results. There was growth of Pseudomonas fluorescens and candida tropicalis colonies. There was no growth in Löwenstein - Jensen and MGIT media of the material taken to rule out tuberculosis lesions (Lupus Vulgaris etc.). Based on the culture antibiogram about result of deep tissue material outcome, the patient was put on Amphotericin-B 3 mg / kg medication.The patient, whose drowsiness gradually increased, had no findings such as neck stiffness and papillary edema that could be otherwise associated with intracranial lesions. Lumbar puncture (LP) was performed to rule out infectious pathologies. In the brain spinal fluid (CSF) examination: no cells were seen, glucose was measured as 60 mg / dl (simultaneous blood glucose: 160mg / dl), protein as 33mg / dl, Cl as 107mmol / l (serum Cl: 88mmol / l). Leukocyte and fungal hyphae were not observed in the CSF gram staining in the sample assessed microbiologically. Punch biopsy was performed under local anesthesia. In the hematoxylin-eosin staining, a large, atypical infiltration that is 2-2.5 times the size of mature lymphocyte was detected in diffuse pattern intertwined with reactive lymphocytes nested within marked necrosis. Immunohistochemical exam detected CD 30 (Focal +), CD20 (+), CD79a (+), MUM1 (+). EBER (+) in situ hybridization was detected. The findings were originally reported in favor of EBER positive DLBCL of nongerminal center in origin with CD30 expression (Figure 4).
DiscussionDiffuse B-cell lymphoma is one of nonepithelial tumors involving the sinonasal cavity. Although its incidence is low, it is an important cause of morbidity and mortality. It constitutes 90% of B-cell lymphomas and may result in progressive growth and mortality depending on its location. It is most common in men over the age of 50. The most commonly reported sites are the maxillary sinus and nasal cavity [6]. EBV infection, autoimmune diseases and family history play a role in its etiology [7]. In our case, previous EBV infection and presence of autoimmune hepatitis were considered as risk factors. Clinical manifestations and physical examination findings of sinonasal lymphomas may be non-specific. In many cases, no specific symptoms or physical examination findings are observed. It becomes impossible for physicians to suspect DLBCL, especially in the absence of specific symptoms, and abnormal physical findings, and even in the absence of B symptoms [8]. They manifest symptoms related to the affected tissue, depending on location. In our case, the absence of B symptoms caused diagnostic challenge, and the condition was associated with SIADH due to the electrolyte imbalance and failure of laboratory exams to improve despite appropriate replacement. Central nervous system involvement in the brain MRI conducted upon noticing this situation and the development of drowsiness in the patient clarifies the etiology of SIADH. Although CT scan has priority in the diagnosis of lymphoma, USG, MRI, CSF cytology, bone marrow aspiration / biopsy, complete blood count, biochemical parameters and serological examinations are recommended to standardize the diagnostic evaluation. Age, stage, serum LDH level, performance status and extranodal involvement are important factors determining the prognosis of lymphoma [5,9]. The prognosis is poor in patients over 60 years of age, those with high serum LDH levels, and patients with more than two extranodal involvement. Serum LDH levels are known to be an independent predictive value in terms of prognosis and survival in cutaneous and systemic lymphomas [10]. In addition, stage III and IV cases also have a poor prognosis based on Ann Arbor staging system [11]. (Table 1). The IPI score obtained by the cumulative evaluation of prognostic factors indicates a low risk for 0-1 points, low-medium risk for 2 points, high-moderate risk for 3, high risk for 4-5 points [12]. In our case, diagnostic CT, MRI and laboratory tests were utilized and the obtained data were assessed in conjunction with clinical information. The IPI score for our case was identified as 5 due to age factor [over 60 years], high LDH level and ECOG performance score, stage [IV] and extranodal involvement. In terms of survival, the prognosis was considered poor. For a long time, chemoradiotherapy has been considered as the main step in DLBCL management. Although the most widely used chemotherapy combination is CHOP [cyclophosphamide, doxorubicin, vincristine, prednisolone] + rituximab; radiotherapy option becomes first line in early-stage tumors of <5 cm in size, elderly patients due to low toxicity, and patients unable to receive chemotherapy due to impaired general condition [13]. In our case, only radiotherapy was administered due to the poor general condition and neurologically, the gradual increase in drowsiness. Conclusıon This interesting case highlights an unusual presentation of sinonasal DLBCL, . Apart from infectious pathologies in lesions involving the nasal vestibule, lymphoma must be considered in the differential diagnosis, histopathological classification should be done, and treatment should be delivered promptly. References
|
|||
| Keywords : Nazal Vestibül , Sinonazal Lenfoma , Uyumsuz ADH Sendromu | |||
|