|
|||||||||
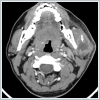
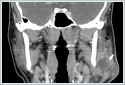
AbstractParotid gland pathologies are clinically significant due to potential involvement of the facial nerve. The facial nerve may be affected by infectious pathologies, trauma, tumors, and iatrogenic causes. Parotid abscesses, which frequently develop in the presence of conditions such as poor oral hygiene, immunosuppression, dehydration, and sialolithiasis, require careful management for this reason. This article presents the case of a 30-year-old immunocompetent male patient with a parotid abscess secondary to blunt trauma. This case is unique in the literature both due to its development following blunt trauma and the isolation of Kocuria kristinae in culture.IntroductionThe parotid gland may be injured either bluntly or by penetration in head and neck trauma. Traumatic parotid pathologies account for 2.5% of all parotid pathologies [1,2]. In injuries occurring at the gland level, the parenchyma is affected, whereas injuries involving the anterior aspect of the gland may involve the Stensen’s duct. The risk of facial nerve involvement in parotid gland injuries makes these pathologies particularly significant [1]. Parotid abscess (PA) typically develops following acute purulent sialadenitis. Reported risk factors for PA include poor oral hygiene, immunosuppression, sialolithiasis, and dehydration. Due to its anatomical relationship with the facial nerve, PA presents a therapeutic challenge [3]. The primary treatment strategy consists of drainage and appropriate antibiotic therapy [3-5]. While the most frequently reported pathogens in PA are Staphylococcus spp., anaerobic bacteria, and Streptococcus spp., numerous other pathogens have also been isolated in PA cases [3,4]. The differential diagnosis of PA also includes sialadenitis, sialolithiasis, soft tissue infections of dental origin, and temporomandibular joint disorders [3-6]. Kocuria kristinae is an aerobic, gram-positive, catalase-positive, coagulase-negative, and non-hemolytic coccus that is part of the skin and oral flora [7-11]. Kocuria kristinae is generally considered to become pathogenic in immunosuppressed patients [7-9,11]. The most common infections associated with Kocuria spp. include bacteremia, skin and soft tissue infections, endophthalmitis, infectious endocarditis, and peritonitis. Recently, an increasing number of Kocuria spp. infections were reported in immunocompetent individuals [11]. In this case report, a patient with parotid abscess secondary to blunt trauma, in which Kocuria kristinae was identified as the causative pathogen, is presented in light of the literature. This is the first reported case in the literature both in terms of its development secondary to blunt trauma and the isolation of Kocuria kristinae in culture. Case ReportA 30-year-old male patient with no known medical history was referred from the Emergency Department to the Otorhinolaryngology clinic due to painful swelling over the mandible. It was learned that five days prior, he had sustained a blunt trauma to the affected area while playing football. The patient reported experiencing pain immediately after the impact, with no mandibular fracture detected upon evaluation in the Emergency Department, and no open wound associated with the trauma. Over the past two days, he had developed swelling in the painful area, with increasing pain intensity. On physical examination, a lesion was observed at the level of the left mandibular angle, characterized by erythema and increased temperature of the overlying skin, as well as tenderness and fluctuance upon palpation (Figure 1).
Trismus was present, with restricted and painful mouth opening of approximately 2 cm. Serous saliva of normal consistency was observed flowing from the Stensen’s duct orifice. No additional significant findings were noted on physical examination. Neck ultrasonography revealed a dense fluid collection of approximately 3×2 cm within the left parotid gland, suggestive of an abscess. To further evaluate potential post-traumatic fractures, the extent of abscess spread, its origin, and involvement of cervical spaces, contrast-enhanced neck computed tomography (CT) was performed. A well-defined collection measuring approximately 3 cm in diameter, consistent with an isolated abscess within the left parotid gland, was observed (Figure 2).
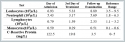
No additional findings were detected on radiological examination. The patient’s blood test results are presented in Table 1.
Informed consent was obtained from the patient for the publication of this case report. DiscussionAlthough PA is considered to be more common in elderly and/or immunosuppressed patients, multiple studies demonstrated its occurrence in healthy individuals across all age groups [3-5]. On physical examination, a fluctuating swelling in the parotid region is the most critical finding suggestive of an abscess. CT or ultrasonography provides sufficient information for the diagnosis of an abscess. When complications are suspected, CT is the preferred imaging modality [4]. Reported complications include facial nerve paralysis, cervicofacial cellulitis, osteomyelitis, temporal lobe abscess, deep neck infections, necrotizing fasciitis, mediastinitis, airway obstruction, and septic shock. Prompt diagnosis and effective treatment are crucial to prevent these complications [3,4]. Abscess drainage can be performed via aspiration or incision [4]. Aspiration drainage is recommended as the initial approach due to its lower risk of facial nerve injury [5]. The recommended duration of antibiotic therapy is generally 10–14 days [3,4]. To date, there are no reported cases of PA secondary to blunt trauma in the literature. Possible etiological mechanisms in our case include the parenchyma becoming susceptible to infection due to the effects of extravasated saliva following trauma or secondary infection of an associated hematoma. Previously, Kocuria spp. was classified as Micrococcus or coagulase-negative Staphylococcus when bacterial typing was performed manually. However, more accurate identification has been achieved with the advances in automated systems [7]. The most commonly used method for identification is VITEK 2 [9,11]. Since this bacterium is generally regarded as a contaminant, its pathogenic potential has often been overlooked. However, in recent years, an increase in both superficial and deep tissue infections caused by Kocuria spp. was reported [7]. Due to phenotypic similarities between Kocuria spp. and coagulase-negative Staphylococcus spp., misidentifications between these genera have occurred. Currently, there are no established treatment guidelines for Kocuria infections, and empirical treatment is initiated in most cases. It was reported that Kocuria spp. is generally susceptible to amoxicillin-clavulanate [11]. In a study by Chaubey et al., infections caused by Kocuria kristinae were evaluated in patients undergoing treatment for head and neck malignancies. In this case series, male patients were predominant, which was attributed to the higher incidence of head and neck cancers in men. Similarly, the mean age was reported as 50.8 years, but this finding was not considered significant on its own. It was demonstrated that Kocuria kristinae infections occur in a wide age range, from neonates to elderly individuals. In the study by Chaubey et al., most patients exhibited leukocytosis and elevated CRP levels [7]. Amina et al. reported a case of meningitis secondary to sphenoid sinusitis in a pediatric patient without immunosuppression, in which Kocuria kristinae was identified as the causative agent. The pathogen was found to be susceptible to penicillin G, amoxicillin, cefotaxime, erythromycin, spiramycin, lincomycin, ofloxacin, pristinamycin, levofloxacin, teicoplanin, and vancomycin, while exhibiting low-level resistance to streptomycin, kanamycin, and gentamicin. The patient was successfully treated with a combination of cefotaxime and vancomycin [8]. Tsai et al. reported a case of a brain abscess caused by Kocuria spp. in a 52-year-old patient with diabetes mellitus. In this case, the pathogen was found to be susceptible to penicillin, cloxacillin, cefmetazole, clindamycin, meropenem, penicillin G, ampicillin/sulbactam, and piperacillin/tazobactam [9]. ConclusionEarly and effective treatment of PA is crucial for preventing complications. Accurate identification of the causative bacterium is essential for appropriate antibiotic therapy planning. With the introduction of advanced technological systems, bacterial classification has become more precise. This has led to the recognition of certain previously overlooked bacteria as causative agents in various infections. A similar situation applies to Kocuria kristinae. AcknowledgementNone. Informed ConsentInformed consent was obtained from the patient for the publication of this case report.References
|
|||||||||
| Keywords : Travma , Künt Travma , Parotis Absesi , Kocuria kristinae | |||||||||
|